About Surrey Colposcopy
About Mr Anil Tailor
Mr Anil Tailor is a senior Consultant Gynaecologist and Gynaecological Oncologist with nearly 35 years of medical experience, including 25 years specialising in gynaecological oncology. He is a recognised expert in colposcopy and cervical screening, offering private consultations and procedures.
A long-standing member of the British Society for Colposcopy and Cervical Pathology (BSCCP) for over 25 years, Mr Tailor has maintained continuous accreditation and remains actively engaged in the latest developments in cervical health through regular attendance at national and international conferences.
In addition to his private practice, Mr Tailor runs busy NHS colposcopy clinics at St Peter's Hospital in Chertsey, where he is known for his thorough, compassionate, and patient-focused approach. His extensive experience enables him to provide rapid, expert assessment and management for patients with abnormal smear results, ensuring timely care and peace of mind.
Read what patients sayAbnormal Smears & Colposcopy
An abnormal cervical smear result does not mean cancer. It usually indicates changes in the cells of the cervix that may need monitoring or treatment.
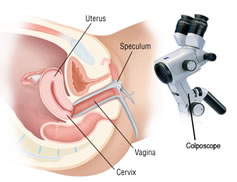
Colposcopy is a straightforward outpatient procedure that allows a specialist to closely examine the cervix using a magnifying device. It helps identify the nature and extent of any cell changes and guides appropriate management.
Most abnormalities are minor and treatable, and early assessment through colposcopy ensures timely care and peace of mind. Watch video
Consulting At:
Mr Anil Tailor holds regular colposcopy clinics at the following leading private hospitals in Surrey:
- Runnymede Hospital
- Guildford Nuffield Hospital
These clinics offer a pleasant, discreet, and safe environment, equipped with modern colposcopy equipment to ensure accurate diagnosis and comfortable care.
Insured & Self-Funding Patients
Almost all insured patients can request to be seen privately under their insurance policy. It can considerably reduce the waiting time. The other advantage is that you will also receive notification of results more promptly.
Smear abnormality and colposcopy procedure is invariably covered in the health insurance unless there is an exclusion for pre-existing abnormality when the policy was started. The policy may have an excess that the patient has to fund. You can request an appointment by filling out the form below.
Self-funding patients can access private care directly without any referral from GP. The fees can be viewed here. You can request an appointment by filling out the form below.
Book a ConsultationVerified Patient Reviews For Colposcopy Services
"I am very grateful for the care and treatment I received from Mr Anil Tailor. From my initial consultation, Mr Anil Tailor was incredibly kind and compassionate, making me feel comfortable and at ease, even during a potentially anxiety-provoking procedure. He took the time to explain everything very clearly, answering all my questions thoroughly and without making me feel rushed. The entire staff was also friendly and helpful, making my experience at the Nuffield hospital truly positive. I highly recommend Mr Anil Tailor and would definitely choose him again for future appointments."
"Mr Tailor put me at ease straight away, was extremely knowledgeable and made time for my questions. Would very much recommend."
"Very professional and took great care in explaining all relevant information."
"Honestly cannot fault my experience in every way. Mr Tailor excelled in all ways - taking time to discuss my situation and answer lots of questions! He made my options clear and made me very comfortable from start to finish. He also took time after my colposcopy to discuss HRT and why I should consider it for proactive reasons. This is the first time this has happened for me and it will definitely result in me taking action. If I do need any further gynaecological treatment or advice in the future Mr. Tailor will be my first choice. So pleased I met him."
"I would highly recommend Dr. Tailor for any check ups & procedures! He is incredibly thorough, knowledgeable, kind & professional. Wonderful service all around!"
"I recently had a LLETZ procedure and coil replacement performed by Dr. Anil Tailor, and I cannot recommend him enough. He was extremely thorough in explaining the entire process, which put me at ease from the start. His calm and reassuring manner made a potentially nerve-wracking experience so much more comfortable. I truly felt in excellent hands throughout the procedure."
"Mr Tailor has exceptional information on everything you need to know & understand about woman’s reproductive system & any concerns. He makes you feel comfortable with asking any questions that come to mind. Highly Recommend."
"I had a very positive experience with Mr Tailor. He was thorough and very considerate. His follow up communication was excellent"
"Really put me at ease during the consultation and provided a good explanation of the process being undertaken and follow up. Any questions I had were already answered before I could even ask them."
Why Choose Surrey Colposcopy Services

Have your procedure in safe hands
Mr Tailor has vast experience in colposcopy and is an accredited member of BSCCP

Find out your results quickly
Mr Tailor uses multiple methods to communicate directly with patients

Reduced hospital visits
Mr Tailor prefers to carry out the colposcopic examination with the consultation

Avoid shortfalls
Mr Tailor is fee-assured by all major insurers and charges within their rates
Fees for Self Funding Patients
You will be charged a fee by Mr Tailor and by the hospital where you are seen. The initial consultation fee for Mr Tailor is £250, and the follow-up consultation fee is £200. There are separate fees for the colposcopy procedure itself, which is £200. Therefore, the fee from Mr Tailor may range from £400 to £450.
The separate fees charged by the hospital for the colposcopy procedure may vary depending on what biopsies are taken and which hospital you are seen at. These additional fees can amount to an extra £600 to £1200.
Therefore, the total fees could range from £1000 to £1650. If you are unsure about what biopsies you may require then you can use the contact form below to explain which hospital you prefer, what smear abnormality you have been found to have, and please specify whether you currently have a contraceptive coil in place as this occasionally needs to be removed if you are going to require a loop biopsy of the cervix. A new coil will immediately be fitted at the same time if you wish but will incur an additional cost from the hospital.
What to Expect at Your Colposcopy Appointment

What Happens at a Colposcopy Consultation?
You will have a brief consultation with Mr Tailor to discuss your medical history, any symptoms you may have, and any relevant past medical or gynaecological history. Smear results will be explained in general terms and your result will be explained in context. You will have the opportunity to ask any questions you may have.
A consent form will be signed before the procedure, ensuring you understand the process and have the opportunity to ask any further questions.
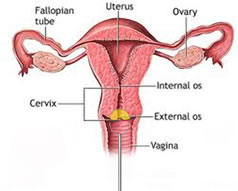
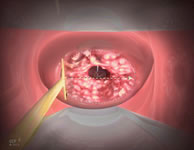
You will then be examined in a private room where a speculum will be inserted into your vagina. A special magnifying instrument called a colposcope will be used to closely examine the cervix. Any mucous or discharge will be gently removed with a mild vinegar-like solution so the surface can be seen clearly and the abnormal precancerous areas will appear white.
This whole process is usually well-tolerated and takes about 5-10 minutes.
What is a Punch Biopsy?
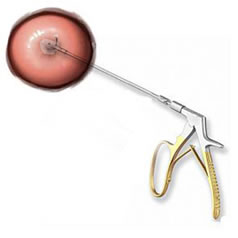
A punch biopsy involves taking a tiny sample of tissue from the cervix using a small instrument. This is usually quick and may cause a brief pinching sensation. The sample is sent to the laboratory for further analysis to confirm if the smear result is correct and help determine the best course of action.
There are usually no restrictions following this procedure and you can carry on with the rest of the day as normal.
What is a Loop Biopsy?
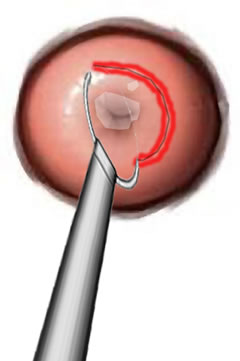
A loop biopsy (also called LLETZ) uses a thin wire loop with an electric current to remove a small area of abnormal cells from the cervix. This is a quick procedure performed under local anaesthetic and is highly effective in treating cell changes. This procedure takes an additional 5 to 10 minutes. It is associated with minimal discomfort and is usually well-tolerated. You may experience some cramping similar to period pain during the procedure, which can be managed with over-the-counter pain relief.
There are some do's and don'ts as explained below. Watch the video about what a loop biopsy or LLETZ is.
How Long Do the Results Take?
Results from biopsies are typically available within 1–2 weeks. Smear results usually take about 2 weeks. You will be contacted directly with your results and any recommendations for further care or follow-up.
Are There Any Do's and Don'ts After the Procedure?
- Usually no restrictions following a colposcopic examination or a punch biopsy.
- After a loop biopsy, avoid heavy exercise and swimming for about 2 to 3 weeks.
- Similarly, refrain from using tampons or having intercourse for 4 weeks after loop biopsy.
- Contact Mr Tailor if you experience heavy bleeding, severe pain, or signs of infection. With very heavy bleeding you may need to go to A&E for urgent assessment.
Frequently Asked Questions
What does an abnormal smear mean?
An abnormal cervical smear means there are changes in the cells of your cervix. This does not mean cancer, but further tests such as a colposcopy may be needed to check for precancerous cervical cells or HPV infection. Watch the video about what abnormal smears mean.
Should I worry about abnormal cervical smear?
Most abnormal smear results are due to minor cell changes and are easily treatable. Early detection and treatment prevent problems later. Your specialist will explain your results and next steps.
How is HPV treated after abnormal smear?
HPV itself is not treated directly, but cell changes caused by HPV (such as CIN 1, CIN 2, CIN 3) can be monitored or treated with procedures like LLETZ if needed. Watch the video about HPV.
What to expect after a colposcopy?
Most people can return to normal activities after a colposcopy. If a biopsy or LLETZ is performed, you may have mild discomfort or light bleeding for a few days. Follow your specialist's aftercare advice.
Can abnormal smear results go back to normal?
Yes, many minor cell changes return to normal without treatment, especially in younger women. Regular follow-up is important to monitor any changes.
Is colposcopy painful?
Colposcopy is usually not painful, though you may feel mild discomfort similar to a smear test. Local anaesthetic is used for biopsies or LLETZ procedures. Watch the video about what colposcopy examination involves.
How long does it take to recover from LLETZ?
Most people recover from LLETZ within 2-4 weeks. Avoid heavy exercise, swimming, tampons, and intercourse for 4 weeks to allow healing.
Watch My YouTube Videos on Abnormal Smears & Colposcopy

This video highlights the critical role of regular cervical smears in preventing cervical cancer. It explains that the primary goal of screening is to detect pre-cancerous changes in cervical cells, which are far easier to treat than cancer itself. Women aged 25 to 64 in England are routinely invited for screening, with intervals based on age. The procedure involves collecting cervical cells to test for high-risk HPV, the virus responsible for most cervical cancers.
It also addresses common concerns and misconceptions, such as why younger and older women may not need screening, and emphasizes that even vaccinated women should continue regular smears. Despite its importance, uptake remains low due to factors like embarrassment or lack of time.

In this video, viewers are reassured that an abnormal cervical smear result usually signifies pre-cancerous changes rather than cancer. It describes how abnormalities are graded, from borderline to severe, and highlights that all of them are treatable, with low-grade changes frequently just needing to be monitored. In order to inform follow-up care, the video also explains how labs check for cell abnormalities and test for high-risk HPV.
Depending on the cytology results and HPV status, management may involve colposcopy or repeat smears. Early intervention is crucial because ignoring abnormal results can cause precancerous cells to develop into cancer. The key to avoiding serious consequences is keeping follow-up appointments.

A thorough introduction to the Human Papilloma Virus (HPV), including information on its types, dangers, and connection to cervical cancer, is provided in this video. It explains that infection is common and frequently symptomless, and that high-risk HPV types, particularly 16 and 18, are the cause of most cervical cancers. High-risk HPV, which can cause precancerous changes, is found by cervical smears.
The effectiveness of HPV vaccinations, especially Gardasil 9, which guards against multiple high-risk types and dramatically lowers the risk of cervical cancer, is also covered in the video. Even after a previous infection or abnormal smear results, vaccination is still beneficial, and routine cervical screening is still necessary.

The significance of cervical smears in detecting precancerous alterations before they worsen is emphasised in this video, which also discusses the distinction between cervical pre-cancer and cervical cancer. It describes how pre-cancer begins in the lower layers of the cervix and progresses gradually over years, possibly leading to cancer if left untreated. Smears are intended to detect these early alterations so that straightforward and efficient treatment is possible.
Only high-grade pre-cancer cases usually require intervention; pre-cancer is rated from low to high. Staging establishes the degree of spread and directs treatment choices if pre-cancer develops into cancer. Smears for early detection can greatly enhance results and avoid invasive procedures.

The grading of abnormalities, the function of colposcopy, and the loop biopsy technique are the main topics of this video, which describes how abnormal cervical smear results are handled. Smears are categorised as borderline to severe, with high-grade changes usually necessitating treatment and low-grade changes frequently monitored. Colposcopy helps to uncover any hidden high-grade abnormalities by closely examining the cervix and validating smear results.
Under local anaesthesia, a loop biopsy is carried out to remove the afflicted area using a fine wire in cases of confirmed high-grade changes. In general, the procedure is well-tolerated and swift. A timely and precise evaluation guarantees the right course of treatment and aids in halting the development of cervical cancer.

By addressing common concerns and explaining the process, this video aims to reassure viewers about what a colposcopy entails. Often performed after an abnormal smear result, a colposcopy uses magnification to examine the cervix closely in order to identify precancerous changes. A speculum is used to view the cervix, and abnormal areas that appear white are highlighted with a mild vinegar solution.
Although there may be some discomfort, the examination usually takes a few minutes and doesn't require anaesthesia. To verify the existence of higher-grade abnormalities, a tiny biopsy might be performed if required. The biopsy's findings inform subsequent care, which may involve treatment like a loop biopsy or monitoring.
The loop biopsy technique, commonly referred to as LLETZ, is described in this video. It is frequently used to treat high-grade precancerous cervical abnormalities. It is usually done during a colposcopy, in which the afflicted tissue is removed using a thin wire loop after a local anaesthetic has been administered. The entire procedure takes about five minutes, after which the area is cauterised to stop the bleeding.
To lower the risk of infection, patients are instructed to refrain from using tampons and sexual activity for four weeks following the procedure. For a few weeks, there may be mild bleeding or discharge. With an 85–90% success rate, the treatment is very effective and, unless several procedures are done, presents little risk to subsequent pregnancies.

The impact of abnormal cervical smears, colposcopy, and procedures like loop biopsies on fertility or pregnancy outcomes is covered in this video. The audience is reassured that HPV infections and abnormal smears do not affect fertility or raise the risk of miscarriage or premature labour. Co-infections like chlamydia can impact fertility, even though HPV is widespread and safe for reproductive health.
It explains that colposcopy is a quick, safe procedure that poses minimal to no risks, even when done during pregnancy. Although deeper procedures may marginally increase the risk of late miscarriage or preterm labour, loop biopsies, which are used to treat high-grade abnormalities, are generally safe when performed shallowly. By keeping an eye on low-grade changes and saving treatment for high-grade abnormalities, modern methods seek to maintain cervical integrity.

